Use of AI to redirect school-aged children during screen time
A study that measured the time spent using digital screens by schoolchildren and adolescents found that the two age groups are spending more time using electronic tablets compared with preschool children. In addition, the lighting conditions were inadequate during the time the children were engaged in use of the screens.1
The study first authors, Jifang Wang, PhD; Yang Shen, MD, PhD; and Jing Zhao, MD, PhD, pointed out that the convenience and efficiency of the various electronics available, i.e., desktop and laptop computers, digital TVs and smartphones, prolong the time that students are engaged in their use, which leads to video display terminal syndrome.2-4
The researchers are from the Eye Institute and Department of Ophthalmology, Eye & ENT Hospital, Fudan University; NHC Key Laboratory of Myopia, Fudan University, Key Laboratory of Myopia, Chinese Academy of Medical Sciences; Shanghai Research Center of Ophthalmology and Optometry; and Shanghai Engineering Research Center of Laser and Autostereoscopic 3D for Vision Care, all in Shanghai, China.
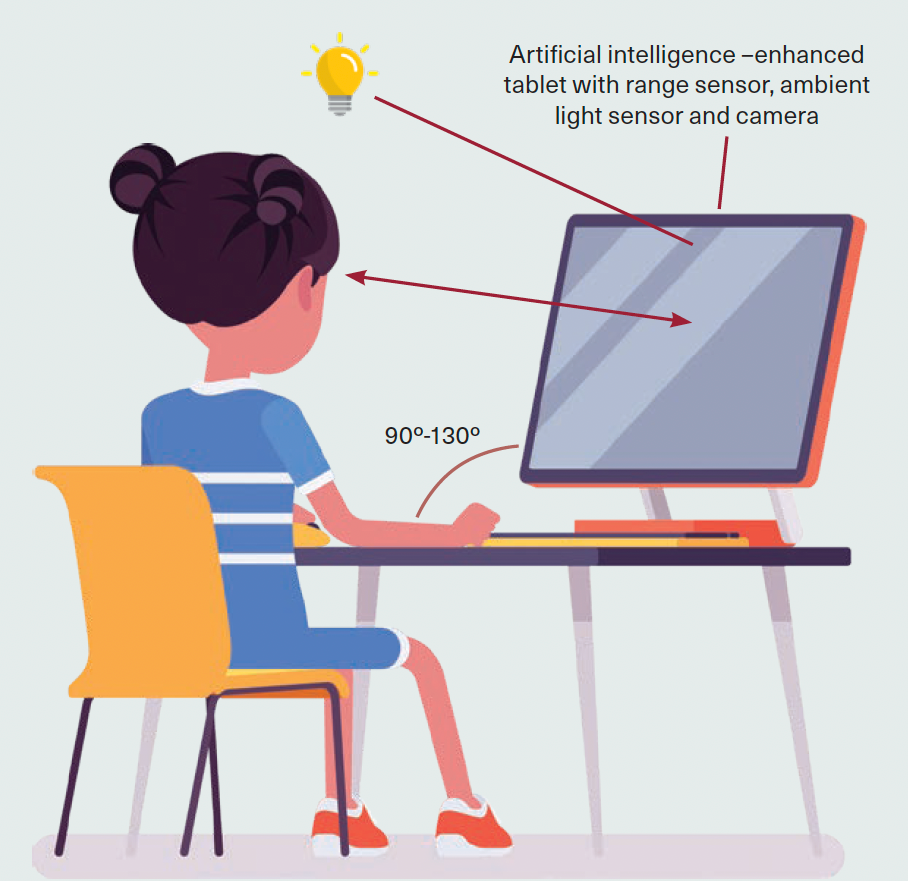
FIGURE 1. An artificial intelligence–enhanced tablet measures
viewing distance, posture, ambient illumination and color temperature.
The COVID-19 pandemic led to remote education, telecommuting, and online entertainment and markedly increased the development of myopia globally.4-6
Environmental factors, such as increased digital screen time, near work, limited outdoor time and dim-light exposure pose significant risks of myopia onset and progression in children and adolescents, aside from genetic factors,7,8 the investigators explained. In addition, using digital screens at a short distance, with poor posture, under poor illumination, or improper color temperature increases the incidence of myopia,9,10 strabismus,11 anisometropia,2 postural scoliosis12 and abnormalities in musculoskeletal development among youth.13
Study design
The authors evaluated how well artificial intelligence (AI)–based alerts worked to modify screen-time practices among the children. The investigators conducted a cross-sectional analysis using data obtained from 6,716 children and adolescents who used commercially available AI-enhanced tablets (Figure 1.) that monitored and recorded their behaviour and environmental light during usage.
The study tested how well the AI-based visual and audible alerts worked to change screen-time behaviour in the study participants.
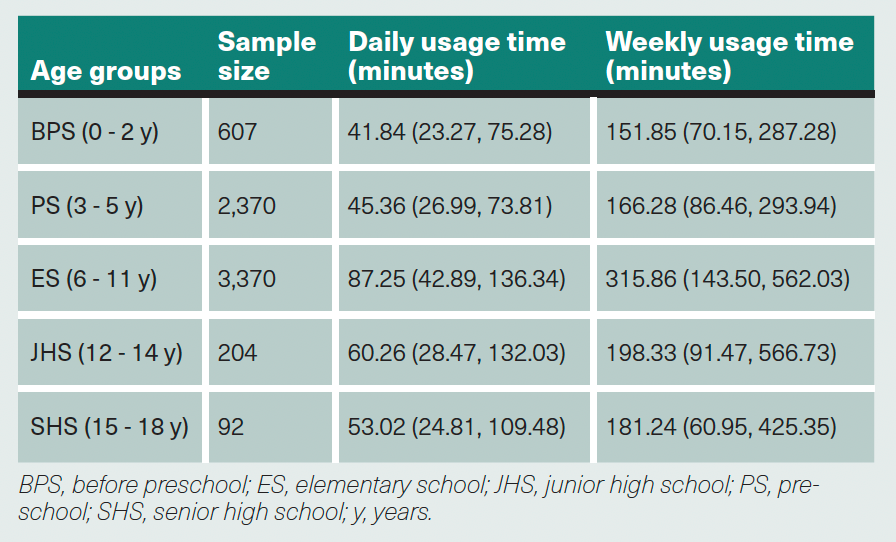
Table. Daily and Weekly Usage Time of Each Group With Median.
Behavioural changes
The investigators reported that the children were engaged in using electronic devices for a median of 58.82 minutes daily.
The elementary school students used the devices the longest, with a median time of 87.25 minutes daily and more than 4 hours weekly. Children under 2 years of age used the devices for a median of 41.84 minutes daily (Table).
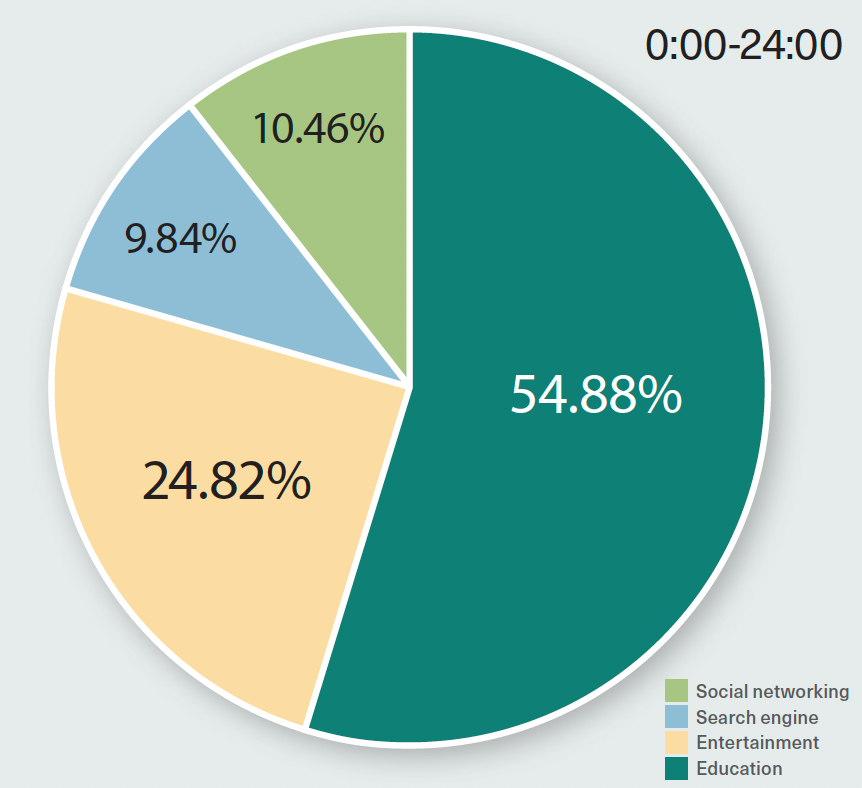
The participants were engaged in learning activities for 54.88% of their screen time (Figure 2.); 51.03% of participants used their tablets for 1 hour at an average distance of less than 50 cm. The AI distance and posture alarms were triggered 807,355 and 509,199 times, respectively.
Figure 2. Percentages of content viewed at different times of the day (social networking, search engine, entertainment, and education).
(Images courtesy of Wang J, Shen Y, Zhao J, et al.)
Regarding environmental lighting, most of the children, 70.65%, were in illumination that was less than 300 lux during the day, and at night 61.11% of the illumination was less than 100 lux. The ambient light for 85.19% of the participants exceeded 4,000 K color temperature during the night.
The authors found that when the AI-based notifications were activated, most of the participants rapidly corrected their viewing habits, i.e., 65.49% in viewing distance and 86.48% in viewing posture (P < .05 for all comparisons).
The study concluded that AI-based notifications are effective for monitoring the time, content and light environment during screen time and for reminding children and adolescents to correct their poor posture and behaviour. The authors advised that more research should be conducted and perhaps adopt “more rigorous sampling techniques, extended monitoring and observation periods, and the inclusion of supplementary online reporting for comprehensive data collection.” They also suggested gathering data that reflect the time spent using other electronic devices, among other relevant factors.
References
1. Wang J, Shen Y, Zhao J, et al. Algorithmic and sensor-based research on Chinese children’s and adolescents’ screen use behavior and light environment. Front Public Health. 2024;12:1352759. doi:10.3389/fpubh.2024.1352759
2. Kaur K, Gurnani B, Nayak S, et al. Digital eye strain- a comprehensive review. Ophthalmol Ther. 2022;11(5):1655-1680. doi: 10.1007/s40123-022-00540-9
3. Feng D, Lu C, Cai Q, Lu J. A study on the design of vision protection products based on children’s visual fatigue under online learning scenarios. Healthcare (Basel). 2022;10(4):621. doi: 10.3390/healthcare10040621
4. Wang G, Zhang Y, Zhao J, Zhang J, Jiang F. Mitigate the effects of home confinement on children during the COVID-19 outbreak. Lancet. 2020;395(10228):945-947. doi:10.1016/S0140-6736(20)30547-X
5. Chang P, Zhang B, Lin L, et al. Comparison of myopic progression before, during, and after COVID-19 lockdown. Ophthalmology. 2021;128(11):1655-1657. doi:10.1016/j.ophtha.2021.03.029
6. Wang J, Li Y, Musch DC, et al. Progression of myopia in school-aged children after COVID-19 home confinement. JAMA Ophthalmol. 2021;139(3):293-300. doi:10.1001/jamaophthalmol.2020.6239
7. Morgan IG, Wu PC, Ostrin LA, et al. IMI risk factors for myopia. Invest Ophthalmol Vis Sci. 2021;62(5):3. doi:10.1167/iovs.62.5.3
8. Ku PW, Steptoe A, Lai YJ, et al. The associations between near visual activity and incident myopia in children: a nationwide 4-year follow-up study. Ophthalmology. 2019; 126(2):214-220. doi: 10.1016/j.ophtha.2018.05.010
9. Yang GY, Huang LH, Schmid KL, et al. Associations between screen exposure in early life and myopia amongst Chinese preschoolers. Int J Environ Res Public Health. 2020;17(3):1056. doi:10.3390/ijerph17031056
10. Hinterlong JE, Holton VL, Chiang CC, Tsai CY, Liou YM. Association of multimedia teaching with myopia: A national study of school children. J Adv Nurs. 2019;75(12):3643-3653. doi:10.1111/jan.14206
11. Németh J, Tapasztó B, Aclimandos WA, et al. Update and guidance on management of myopia: European Society of Ophthalmology in cooperation with International Myopia Institute. Eur J Ophthalmol. 2021;31(3):853-883. doi:10.1177/1120672121998960
12. Nault ML, Allard P, Hinse S, et al. Relations between standing stability and body posture parameters in adolescent idiopathic scoliosis. Spine (Phila Pa 1976). 2002;27(17):1911-1917. doi:10.1097/00007632-200209010-00018
13. David D, Giannini C, Chiarelli F, Mohn A. Text neck syndrome in children and adolescents. Int J Env Res Public Health. 2021;18(4):1565. doi:10.3390/ijerph18041565

Newsletter
Join ophthalmologists across Europe—sign up for exclusive updates and innovations in surgical techniques and clinical care.