Potential for achieving broader range of vision with a monofocal IOL – Preliminary findings in patients implanted with the ZEISS CT LUCIA 621P® IOL
In today’s digital society and with many older adults still working and keeping active, daily life for patients in the cataract surgery population often involves vision in the far to intermediate range. Perfect vision may not be necessary to perform many of these activities, and we can expect that most people will be happy to have a level of vision that allows them to function without needing glasses.
Several options exist for providing patients with a range of functional vision for completing their everyday activities without refractive correction. Recently, certain monofocal IOLs with modified aspheric profiles, so-called monofocal+ or enhanced monofocal IOLs, have been introduced with optical designs that are intended to slightly extend the range of vision into the intermediate range. Out-of-pocket cost to patients in countries where reimbursement is lacking can sometimes be a barrier to use of the latter technologies.1 Corresponding with that issue is surgeon’s concern about achieving patient satisfaction considering that an increase in patients’ outcomes expectations accompany increasing financial burden.
With this information in mind, we were struck by hearing volunteered reports of less need for spectacles postoperatively over a broader than expected distance range from patients we implanted with the monofocal aspheric, hydrophobic CT LUCIA 621P IOL (Carl Zeiss Meditec AG) in the setting of a clinical study performed during a cataract surgery mission trip. We decided to investigate this finding further through defocus curve testing. As described below, the defocus curve results corroborated the subjective reports by showing that the CT LUCIA 621P extended the range of focus, if the refraction was shifted in the myopic direction.
Clinical study outcomes
We regularly volunteer for international missions to Cambodia through the Khmer Sight Foundation NGO and the Augenärzte für die Welt gGmbH NGO to perform cataract surgery and train local ophthalmologists. During a trip in the spring of 2022, we agreed to conduct a study sponsored by Carl Zeiss Meditec AG to evaluate outcomes of surgery using the CT LUCIA 621P and the IOLMaster 700 (Carl Zeiss Meditec AG) for biometry and IOL power calculations.
We gladly agreed to this project because we believed that features of both technologies could contribute to better outcomes in the challenging situation of mission surgery. With the IOLMaster 700, preoperative biometry could be done with greater efficiency and accuracy as compared with A-scan, which is typically used. Further increasing efficiency and adding safety, the CT LUCIA 621P comes fully preloaded in a proprietary single-use injection system (BLUESERT™).
Our study enrolled patients with clinically significant (Lens Opacities Classification System III grade ≥ 3), relatively dense senile cataract who had the potential to achieve corrected distance visual acuity (CDVA) 0.3 logMAR or better, were deemed suitable for undergoing extracapsular cataract extraction via phacoemulsification followed by implantation of a posterior chamber IOL with a calculated power between +4.0 D and + 34.0 D and were expected to return for scheduled follow-up at 1 and 3 months postoperatively.
We operated on 81 eyes of 52 patients who had a mean age of 68.3 years and mean preoperative CDVA 0.58 logMAR. Outcomes data from the 3-month postoperative visit were remarkable both with respect to the attendance rate and functional results. We examined 79 eyes (98%) at 3 months, and they all achieved monocular CDVA ≥ 0.3 logMAR or better. LogMAR CDVA averaged 0.05 ± 0.07 and was 0.1 (20/25) or better in 67 eyes (85 %) and 0.0 (20/20) or better in 46 eyes (58 %). Furthermore, we saw no evidence of IOL glistenings, poster capsular opacification (PCO), or significant IOL decentration.
We returned to Cambodia a year later, and during that trip we saw some patients operated on during our study. On examining these patients, we found they had no evidence of PCO and learned that many were functioning well without glasses. After obtaining monocular defocus curves in a few patients that indeed showed they had an extended range of focus, the original study protocol was amended to include longer term follow-up visits with defocus testing.
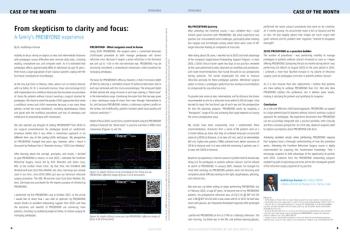
We performed defocus testing in 30 eyes of patients seen approximately 14 months postoperatively. All of the eyes tested had CDVA of 0.2 logMAR or better with a mean post-op refraction of -0.3 D spherical equivalent (SE). For comparability, best corrected, with zero residual refraction for distance VA, defocus measurements were performed on these eyes. To simulate the patients' subjective perception, the best corrected defocus curve was shifted to a myopic outcome (-0.5 D).
As shown in Figure 1, these slight myopic eyes achieved VA results across defocus levels that simulate an extended range of vision. In fact, it seems to us that the slightly myopic CT LUCIA 621P defocus curve is similar to that shown for current monofocal+ IOL models. 2,3
Discussion
In examining patients who returned 14 months after surgery we found that they achieved a slightly myopic outcome. Yet, few patients were requesting spectacles. This clinical finding is consistent with the results of our defocus testing that showed the CT LUCIA 621P provided a certain range of uncorrected vision in cases with slightly myopic outcomes.
Contrary to what surgeons might expect, shifting the refractive outcome to a slightly myopic value does not necessarily cause patients to perceive decreased distance VA. In our patient population, this shift in the defocus curve would give patients a “depth of focus” of nearly 2 diopters, while maintaining good distance VA.
Findings of a recently published prospective clinical study showed that the CT LUCIA 621P provided excellent visual and refractive outcomes and good quality of vision.4 We believe that these properties combined with the optical quality of the CT LUCIA 621P biomaterial are essential to achieve above reported outcomes with a slight myopic shift. Achieving this type of result for individual patients will also depend on the sphericity of their cornea and centration of the IOL to ensure that the lens will provide the intended benefits of its optical design.
Conclusion
Obtaining excellent results that are maintained over time is important when performing cataract surgery in developing countries where access to future ophthalmic care can be poor. An outcome that provides patients with a functional range of uncorrected vision is also highly desirable considering that obtaining spectacles can be difficult for these individuals.
The results from our study involving a challenging mission surgery patient population show that we reached the above mentioned goals in procedures performed using the ZEISS IOLMaster 700 and ZEISS CT LUCIA 621P. Our patients achieved impressive functional results as demonstrated by our primary endpoint analysis of CDVA at 3 months postoperatively, and the unanticipated benefit of a broader range of functional vision with logMar VA of 0.3 or better up to defocus level of nearly -2.0 D if the refraction would slightly be shifted in the myopic direction as documented by both subjective reports and objective defocus testing.
References
- ESCRS Clinical Trends Survey 2022. EuroTimes. IME Supplement, September 2023. https://www.escrs.org/media/5cbb4kx4/2022_escrs_clinical-surveysupplement. pdf. Accessed November 28, 2023.
- Yangzes S, Kamble N, Grewal S, Grewal SPS. Comparison of an asp heric monofocal intraocular lens with the new generation monofocal le ns using defocus curve. Indian J Ophthalmol. 2020;68(12):3025-3029.
- Auffarth GU, Gerl M, Tsai L, et al; Quantum Study Group. Clinic al evaluation of a new monofocal IOL with enhanced intermediate function in p atients with cataract. J Cataract Refract Surg. 2021;47(2):184-191.
- García-Tomás B, Marín-Sánchez JM, García-Elskamp C, et al. Clin ical outcomes of a monofocal, optimized, aspheric, hydrophobic acrylic intrao cular lens implant. Clin Ophthalmol. 2023;17:3215-3224.
Dr Kretz is Managing Director at the Precise Vision Augenärzte, Headquarter, Rheine, Germany and CEO of the German NGO Augenärzte für die Welt gGmbH, Rheine, Germany.
Professor Shah is a Consultant Ophthalmic Surgeon at the Birmingham and Midland Eye Centre, Birmingham, UK.
Newsletter
Get the essential updates shaping the future of pharma manufacturing and compliance—subscribe today to Pharmaceutical Technology and never miss a breakthrough.