Optimizing diagnosis and surgical management of diabetic retinopathy using advanced imaging technologies
Diabetic Retinopathy ranked as the fifth most common cause of blindness among adults aged 50 and older in 2020 according to data from the Global Burden of Disease study. Aude Couturier, MD shares her experience of using advanced imaging technologies to optimize diagnosis and surgical management of her DR patients in our latest Case of the Month.
This article is dedicated to the memory of Ramin Tadayoni, MD, PhD.
Data from the Global Burden of Disease Study showed that in 2020, diabetic retinopathy (DR) ranked as the fifth most common cause of blindness and moderate and severe vision impairment among adults aged 50 years and older.1 Despite advances in medical/pharmacologic therapy for achieving systemic metabolic control and for managing diabetic eye disease, the burden of these consequences of DR may be expected to increase in association with population aging and as the prevalence of diabetes continues to rise.2
Surgical intervention with vitrectomy is required for the management of some vision-threatening complications of proliferative DR, including tractional retinal detachment involving or threatening the fovea, persistent vitreous hemorrhage, mixed retinal detachment, and tractional diabetic macular edema. The surgical goals include relieving traction, removing fibrovascular proliferation and the posterior hyaloid, and ensuring retinal attachment with tamponade as needed. Determining the need and urgency for performing vitrectomy and achieving optimal functional and anatomical surgical outcomes depends on the ability to visualize the pathology. Developments in technologies for diagnostic imaging and surgical visualization enable clinicians to make informed decisions by visualizing pathology, and subsequently improving patient outcomes.
Advances in preoperative imaging
In addition to establishing the indication for surgery, findings on preoperative imaging are used for planning the procedure and have prognostic significance. Referral to preoperative images facilitates location of interventional targets, and there is accumulating evidence demonstrating that certain features in eyes with DR are predictors for risk of DR progression and visual outcome.
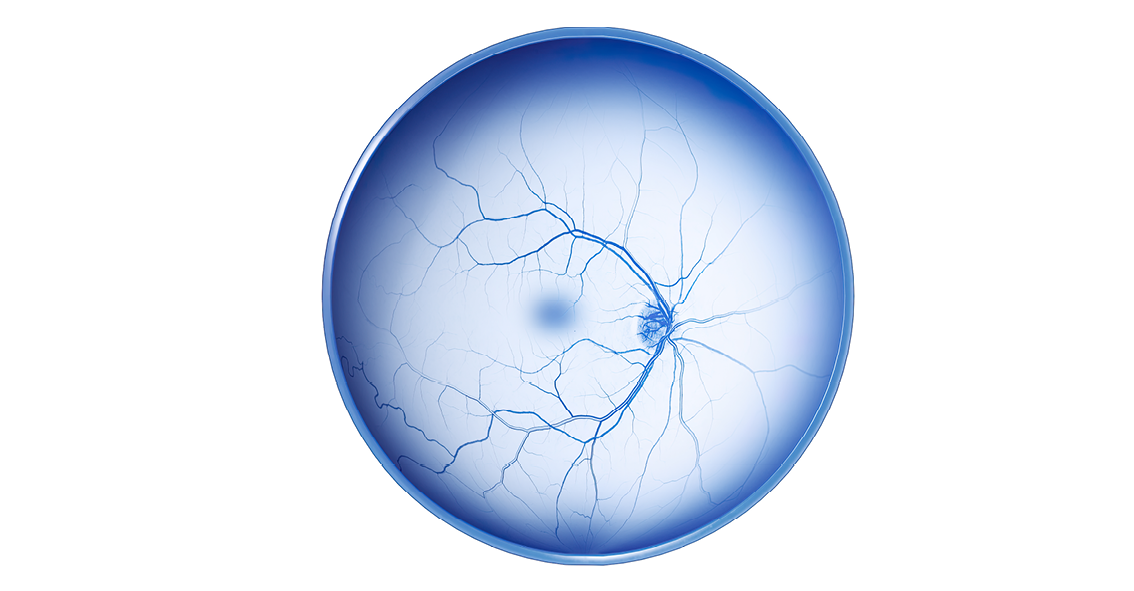
Color fundus photography (CFP) has been the mainstay for evaluating eyes with DR. However, the 7-standard ETDRS fields provide a limited field of view (75°) and fail to capture pathology existing in the peripheral retina, which has become of significant importance for predicting progression of DR.3 In addition, visualization of the fibrovascular proliferation and its extension beyond the mid-periphery is critical for planning surgery in eyes with tractional retinal detachment (Figure 1). Currently available dedicated widefield and ultra-widefield camera systems provide single capture FOVs beyond the 7-field ETDRS area offering acquisition efficiency, enhanced patient comfort, and view beyond the mid-periphery. The ZEISS CLARUS is one such UWF fundus camera with a FOV of 133° for a single image and up to 267° with ultra-wide field montage.
In addition to CFP, optical coherence tomography (OCT) is a cornerstone in the evaluation and management of diabetic eye disease. OCT provides high resolution images of retinal morphology and relevant DR lesions that makes it a valuable aid in establishing the need for medical or surgical intervention and procedure planning. The detailed OCT images can also allow detection of pathology that can be overlooked on the color fundus photographs, such as small retinal breaks or areas of fibrovascular proliferation. OCT biomarkers such as Disorganization of the Retinal Inner Layers (DRIL) are also important for determining visual prognosis and treatment response of patients with diabetic macular edema (DME).4,5
When used together, quality images from CFP and OCT enable understanding of the extent of proliferation and the connection of the posterior hyaloid to new vessels. Surgically this is important to understand where to initiate opening in the posterior hyaloid face.
Used to assess retinal vasculature, fluorescein angiography (FA) has also been a key diagnostic tool for imaging eyes with DR, and its utility has expanded with the development of widefield and ultra-widefield technologies. Nevertheless, FA is an invasive technique that carries risks and is contraindicated in certain patients. Furthermore, FA has limited depth resolution, and obtaining good quality images depends on operator expertise.
OCT angiography (OCTA) is a noninvasive study that provides depth-resolved images of the retinal microvasculature without need for a highly trained operator. However, OCTA does not identify leakage, and so it serves as a complement to FA rather than an alternative. OCTA is especially important for visualizing changes to the foveal avascular zone (FAZ), retinal ischemia, and changes to the vascular density that are difficult to detect and quantify on FA (Figure 1). These OCTA biomarkers provide diagnostic, prognostic, and predictive information related to visual outcome, risk of progression, and response to treatment (intravitreal steroid or anti-VEGF).6
Advances in intra-operative visualization
Obtaining maximal visualization intraoperatively is critical to the success of vitrectomy performed for complications of proliferative diabetic retinopathy (PDR). The utilization of a microscope-integrated intraoperative OCT (iOCT) is very crucial as it addresses this need by enhancing identification of existing pathology and allowing surgeons to operate with greater safety and precision near the retina.
Use of a heads-up three-dimensional (3D) digital viewing system, such as the ZEISS ARTEVO 800 or its successor, the ZEISS ARTEVO 850, also provides benefits when performing vitrectomy for complications of DR. The 3D digital visualization offers enhanced resolution, magnification, and depth of field, with the latter having particular value in cases where the fibrovascular proliferation is attached to the posterior pole. This technology also allows the operation to be performed with a lower light intensity that results in less glare for the surgeon and less risk of phototoxicity for the patient. Moreover, surgeons benefit from the ergonomic advantages of using a heads-up display.
The following cases involving patients with PDR illustrate how I use advanced imaging technologies to help me with diagnosis, surgical planning, and intraoperative decision-making.
Case example 1
A 29-year-old patient presented with significant vision loss in the left eye. On examination she was found to have 20/200 BCVA associated with tractional retinal detachment. The B scan OCT image showed vast fibrovascular proliferation along the arcade and traction on the macula. The patient was scheduled for surgery (Figure 2).
Video 1 Case example 1: Surgical management of a patient with proliferative diabetic retinopathy.
iOCT was used to confirm the planned site for opening the posterior hyaloid, guided its removal from sites of attachment to the posterior pole and the midperiphery, and used to verify absence of residual hyaloid (Video 1).The intraoperative imaging also revealed new vessels attached to the fovea border that made careful dissection mandatory for optimizing functional results. With good visualization, I was able to complete the dissection without causing any intraoperative breaks and therefore avoid the need for tamponade.
Case example 2
A second case also involved a relatively young patient with type 1 diabetes found to have proliferation of new vessels primarily on the optic nerve head but also along the major vascular arcades. Earlier intravitreal injection of an anti-VEGF agent increased traction on the retina. Therefore, it was crucial to find the space between the retina and the proliferation for opening the posterior hyaloid and to remove the proliferation without inducing traction while minimizing the risk for causing a break. Using iOCT after completing the dissection of the new vessels allowed me to check the status of the macula and confirm absence of a break (Figure 3).
Conclusion
Quality pre-operative imaging is essential for determining the surgical indication and treatment plan in eyes with PDR. Precise analysis of the extension of the fibrovascular proliferations and of the attachment to the posterior hyaloid serves as a guide to surgical decision-making. In the same way, iOCT associated with a high-resolution digital microscope has a valuable role in the effectiveness and safety of these delicate surgeries where accurate identification of dissection planes and the absence of iatrogenic dehiscence is crucial for achieving success.
References
- GBD 2019 Blindness and Vision Impairment Collaborators; Vision Loss Expert Group of the Global Burden of Disease Study. Causes of blindness and vision impairment in 2020 and trends over 30 years, and prevalence of avoidable blindness in relation to VISION 2020: the Right to Sight: an analysis for the Global Burden of Disease Study. Lancet Glob Health 2021;9(2):e144-e160.
- Teo ZL, Tham YC, Yu M, et al. Global prevalence of diabetic retinopathy and projection of burden through 2045: Systematic review and meta-analysis. Ophthalmology. 2021;128(11):1580-1591]
- Silva PS, Cavallerano JD, Haddad NMN, et al. Peripheral lesions identified on ultrawide field imaging predict increased risk of diabetic retinopathy progression over 4 years. Ophthalmology. 2015;122(5):949-956.
- Joltikov KA, Sesi CA, de Castro VM, et al. Ophthalmology. 2018;59(13):5481-5486.
- Munk MR, Somfai GM, de Smet MD, et al. The role of intravitreal corticosteroids in the treatment of DME: Predictive OCT biomarkers. Int J Mol Sci. 2022; 23(14),7585.
- Vujosevic S, Cunha-Vaz J, Figueira, J, et al. Standardization of optical coherence tomography angiography imaging biomarkers in diabetic retinal disease. Ophthalmic Res. 2021;64 (6):871-887.
Prof. Aude Couturier is an ophthalmologist at hospital Lariboisière (AP-HP) in Paris. She is specialized in vitreoretinal surgery, treatment of retinal diseases and retinal imaging.
Newsletter
Get the essential updates shaping the future of pharma manufacturing and compliance—subscribe today to Pharmaceutical Technology and never miss a breakthrough.