SMILE for myopia and myopic astigmatism – Increasing procedural ease and efficiency with the VISUMAX 800 femtosecond laser
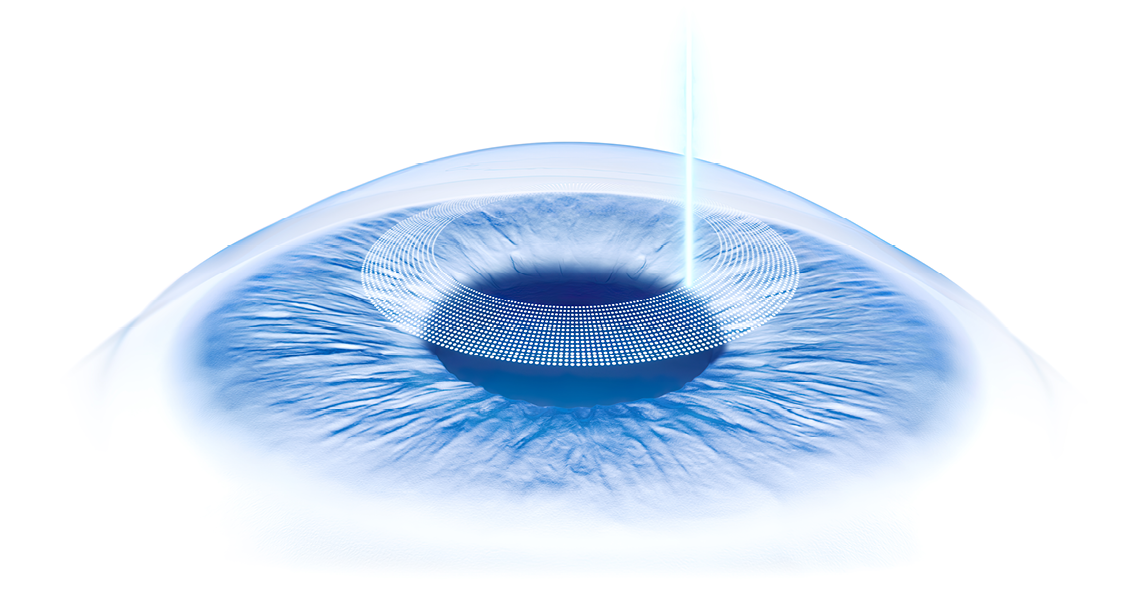
We have been performing SMILE with the VisuMax femtosecond laser (Carl Zeiss Meditec AG; Jena, Germany) for myopia and myopic astigmatism since October 2012, and its outcomes and benefits make it our preferred method of laser vision correction for these cases. SMILE is predictably safe and effective, and its refractive results show good long-term stability, even when treating higher myopia.1 In addition, SMILE has advantages of being a flapless procedure that include possibly less postoperative dry eye and better corneal biomechanics compared to LASIK.1,2,3
In 2021, the VISUMAX 800 (Carl Zeiss Meditec AG) became available as a next generation femtosecond laser, and it is designed with many upgrades. Faster speed is the most noteworthy enhancement found on the VISUMAX 800 that has a 4-fold faster laser repetition rate compared to the VisuMax – 2 MHz vs 500 kHz (Video 1).
Video 1.
In addition, the VISUMAX 800 is equipped with new digital surgeon support functions, including a centration aid (CentraLign®) and a tool to facilitate cyclotorsion alignment (OcuLign®), which comes into effect particularly when correcting higher astigmatism.
Physically and operationally, the VISUMAX 800 differs as well, having separate laser and microscope arms and using heads-up docking that is achieved by lowering the laser onto the eye rather than by raising the bed (Video 2). It also has a smaller footprint than the VisuMax because moving parts are integrated into the laser arms and there is no attached bed. Therefore, the VISUMAX 800 is also mobile, takes up less space in our operating theatre, can be used with various patient beds, and allows for what we believe is a wider, more comfortable environment for patients.
Furthermore, the VISUMAX 800 is part of a digitally connected refractive system that allows for a fully integrated, streamlined workflow. With this feature, treatment planning can be done anywhere surgeons have access to the Internet, and because of the electronic data transfer, data entry only needs to be done once, saving time and reducing the potential for human error.
Video 2.
Testing its attributes
We acquired the VISUMAX 800 in September 2021, believing that it had compelling features that would result in meaningful procedural and clinical improvements. Once we completed what was a short learning curve, we decided to conduct a prospective study to investigate our predictions.
Our study randomized patients undergoing bilateral SMILE for myopia or myopic astigmatism to a procedure using the VisuMax or VISUMAX 800 lasers. As a primary objective we evaluated if the new laser had significant benefits in terms of improving workflow efficiency, but we also looked at clinical outcomes to see if it brought any advantages for enhancing the patients’ intraoperative experience and early visual outcomes.
We enrolled 60 patients with -1.00 to -10.00 D spherical equivalent (SE) and <1.50 D manifest cylinder. Although SMILE can be used to treat up to 5.0 D astigmatism, we excluded eyes with cylinder ≥1.50 D because those eyes would require marking as an additional step that could have affected our assessment of surgical efficiency.
All procedures were performed by Sri Ganesh, MD, using the same nomogram for both groups. Optimized settings were used for each laser. Energy cut index, pulse energy, and side cut spot separation were slightly lower for the VISUMAX 800 versus the VisuMax (26, 135 nJ, and 1.5 μ vs 27, 140 nJ, and 2.0μ). With both lasers, cap cut spot separation was 4.5 μ and lenticule cut spot separation was 4.3 μ. In addition, the workflow differed for the two groups because with its separate swiveling laser and microscope arms, the VISUMAX 800 allowed us to perform immediate bilateral sequential docking and lasering of right and left eyes followed by bilateral sequential lenticule dissection.
Procedures done with the VisuMax were done according to our conventional workflow where the laser treatment and lenticule extraction steps are done sequentially in the right eye and then completed in the left eye. With this approach, raising and lowering of the patient bed are each done an additional time compared to the workflow we followed using the VISUMAX 800. As another difference between our two groups, centration was assisted by the CentraLign function using the VISUMAX 800 but was based on clinician judgment for the VisuMax.
To compare efficiency, we measured docking time (from insertion of eye speculum to completion of laser delivery), lenticule dissection time (from entry of the dissector into the pocket until extraction of the lenticule) and overall surgical time per case (from when the patient sat down on the bed until they got up after the procedure). In addition, Dr Ganesh graded the ease of lenticule separation on a scale of 1 (very difficult/inseparable) to 5 (very easy/effortless). Patients were given a questionnaire for rating pain during the procedure, foreign body sensation (FBS), and their overall experience, and we looked at measures of visual function and quality at postop day 1 and week 2.
Our two study groups were similar with respect to mean age as well as refractive and cornea characteristics. All procedures were completed uneventfully without any intraoperative complications, including suction loss, opaque bubble layer formation, or black spots.
As summarized in the table, we found statistically significant differences favoring the VISUMAX 800 for having a shorter docking time and shorter overall surgical time. Lenticule dissection also took less time in cases performed with the VISUMAX 800, although the difference between groups did not quite achieve statistical significance. However, the surgeon’s grading of lenticule dissection showed it was significantly easier after using the VISUMAX 800 (P <.03).
Scores for the patient questionnaire ratings were similar in the two groups and indicated minimal discomfort and high satisfaction levels overall. Visual acuity and visual quality results were also similar in the two groups.
Personal perspectives
Collectively, our data reinforce the efficacy and safety of SMILE using the VisuMax femtosecond laser and validate our expectations that with its surgeon-supporting systems and technology upgrades, the VISUMAX 800 would improve workflow efficiency. The significant reduction in docking time is accounted for by time saved with the VISUMAX 800 in applanating the eye, achieving centration, and laser delivery. Cutting the lenticule itself takes just 8 to 9 seconds using the VISUMAX 800 compared to 25 to 27 seconds with the VisuMax.
Reduced docking time together with time saved from performing the laser treatments and lenticule dissections as sequential bilateral procedures without having to reposition the bed and arms of the laser and microscope further contributed to the significant reduction in overall surgical time.
We speculate that the slightly lower energy cut index used in the VISUMAX 800 femtosecond laser may have resulted in a smoother bubble pattern that enabled lenticule dissection as measured by the shorter procedure time and better surgeon’s ratings. A smoother bubble pattern might also lead to a smoother lenticule bed that might translate into superior early visual outcomes using the VISUMAX 800 if data were analyzed in a larger population. Similarly, it would be interesting to investigate in a larger study whether the centration guide feature of the VISUMAX 800 improves treatment centration, resulting in less induction of higher order aberrations and better quality of vision postoperatively.
In theory, reduced suction time should lessen the risk for suction loss during SMILE. The rate of suction loss during SMILE with the VisuMax in our practice is just 0.125%. Therefore, it is not unexpected that we encountered no cases of suction loss in our study. Perhaps surgeons who are experiencing a higher rate of suction loss using the VisuMax might find an advantage switching to the VISUMAX 800, and surgeons who hesitated to perform SMILE because of concern that suction loss would occur during the relatively long laser delivery will feel more confident using the VISUMAX 800.
Our learning curve for implementing the VISUMAX 800 related to differences in its operation compared to the VisuMax. With the VISUMAX 800 the laser arms move, not the bed, and application of the laser is tracked via the monitor instead of the microscope.
In addition, with CentraLign and OcuLign, the VISUMAX 800 comes with two new surgeon supporting functions. However, the learning curve was easy and rapidly completed, and for surgeons who are novices to both devices, the surgeon-supporting aids of the VISUMAX 800 might make for a relatively shorter learning curve.
Conclusion
The take-home messages from our study are simple. SMILE with the VisuMax femtosecond laser is an excellent procedure for correcting myopia and myopic astigmatism. Switching to the VISUMAX 800 allows us to continue to deliver great clinical outcomes while offering measurable advantages for improving workflow efficiency.
References
- Shah R. History and results; indications and contraindications of SMILE compared with LASIK. Asia Pac J Ophthalmol (Phila). 2019;8(5):371-376.
- Guo H, Hosseini-Moghaddam SM, Hodge W. Corneal biomechanical properties after SMILE versus FLEX, LASIK, LASEK, or PRK: a systematic review and meta-analysis.
- Denoyer A, Landman E, Trinh L, Faure J-F, Auclin F, Baudouin C. Dry eye disease after refractive surgery: comparative outcomes of small incision lenticule extraction versus LASIK. Ophthalmol.2015;122(4):669-76.
Dr. Brar is a senior consultant at Nethradhama Super Specialty Eye Hospital, Bangalore, India. She is a consultant to Carl Zeiss Meditec AG.
Newsletter
Get the essential updates shaping the future of pharma manufacturing and compliance—subscribe today to Pharmaceutical Technology and never miss a breakthrough.