Corneal refractive surgery for presbyopia: why ZEISS PRESBYOND was our preferred solution
Multiple options are available for managing presbyopia, of which glasses are the most commonly used. Surgical approaches, however, offer an alternative for individuals seeking to reduce spectacle dependence. For patients with a clear lens needing ametropic correction, the surgical options include laser keratorefractive procedures and refractive lens exchange with implantation of a presbyopia-correcting IOL.
We began offering PRESBYOND (Carl Zeiss Meditec AG; Jena, Germany) in 2018 to presbyopic patients without cataract who would like to reduce their spectacle dependence. Among the multiple LASIK techniques available for presbyopic correction, PRESBYOND is our procedure of choice because of its working principle, reported good clinical outcomes, and patient satisfaction.1-4
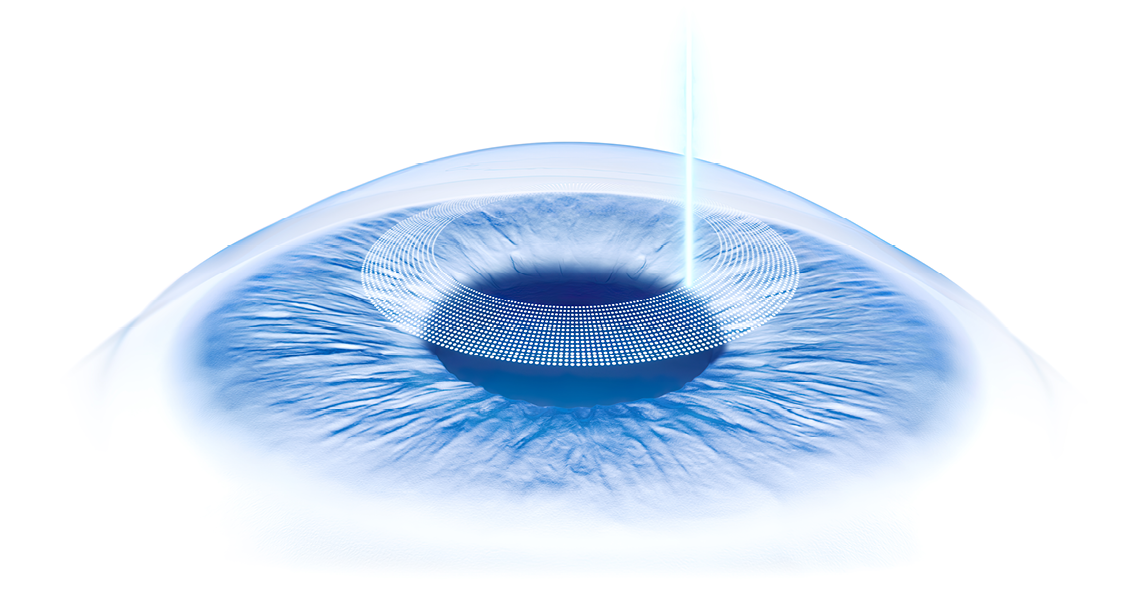
Performed with the MEL 80 or MEL 90 excimer laser (Carl Zeiss Meditec) and proprietary planning software available on the CRS-Master or Refractive Workplace (both Carl Zeiss Meditec), PRESBYOND is a binocular LASIK procedure that can correct ametropias and compensate for presbyopia. Using a non-linear aspheric ablation profile, PRESBYOND induces a small anisometropia of up to -1.5 D. PRESBYOND also controls the amount of spherical aberration in order to achieve an amount within the so-called “therapeutic” range that gives patients increased depth of focus, allowing for continuous focused vision over a range of distances.
Reports published in peer-reviewed journals by multiple surgeons show that PRESBYOND is a safe, well-tolerated, stable, and effective procedure for treating presbyopic patients with myopia and hyperopia, and that it is associated with high rates of spectacle independence, excellent visual quality, and maintenance of contrast sensitivity and functional stereoacuity.1-4
Case history
A 47-year-old soldier suffering from presbyopia presented to our clinic with interest in becoming spectacle independent. He had been referred by another soldier from his unit who was successfully treated at our clinic. The new patient wanted his procedure to be done very soon. He was due to be deployed abroad the next month and said he would face challenges in terms of distance, intermediate, and near vision in his assignment.
Examination showed the patient had a clear lens and moderate myopia with low astigmatism: his refraction was -4.25 D (-0.5 D x 135°) OD and -1.0 D (-0.25 D x 16°) OS. Eye dominance testing showed the patient was left eye dominant, and anisometropia testing showed he tolerated 1.0 D very well. The patient was deemed to be a suitable candidate for PRESBYOND based on additional preoperative assessments that included evaluations of corneal thickness, anterior and posterior corneal surface topography, epithelial thickness, and dry eye disease. Aberrometry showed total spherical aberration (measured in Malacara notation) was -0.37 μm OD and -0.20 μm OS.
Considering the patient’s profession and the associated potential risk for flap displacements, we were also evaluating if a flapless procedure might be a better option for him. However, a surface treatment was out of the question due to the long healing time and other reasons. We were also hesitant to perform SMILE with monovision because the patient had a corneal scar OD from injury with a metal splint.
To give this patient a chance of achieving freedom from glasses, we decided to perform PRESBYOND and accept the risk of flap displacement as LASIK-based procedures are usually indicated for patients of his age. After obtaining his consent, PRESBYOND was performed targeting the non-dominant eye (OD) for -1.0 D and the dominant eye (OS) for plano.
The patient’s refraction at 3 months postop, as shown in figure 1, was -1.25 D OD and 0.0 D OS. Spherical aberration was -0.3 μm OD and -0.4 μm OS. Functional testing showed distance uncorrected visual acuity was 20/40 OD, 20/16 OS, and 20/16 binocularly, and near uncorrected visual acuity was 20/20 OD, 20/25 OS, and 20/20 binocularly.
When seen in our clinic after returning from his stay abroad, the patient seemed highly satisfied. He said that he was able to see from distance to near without any additional correction, and if given the choice, he would undergo the same treatment again.
Discussion
Multiple LASIK procedures have been developed to manage presbyopic patients, including approaches based on creating a multifocal cornea or full monovision. Those approaches, however, suffer from limitations that include reduced quality of vision and contrast sensitivity, loss of stereoacuity, and unacceptable rates of dysphotopsia complaints and ≥ 2-line decreases in CDVA.5,6
With PRESBYOND, a micro-anisometropia is created, making it possible to take advantage of the beneficial effect that spherical aberration within a defined "therapeutic" range has on depth of focus. As demonstrated by Rocha et al. in a study using adaptive optics, depth of focus increased when either positive or negative spherical aberration was adjusted (increased or decreased) to be in the range of ± 0.3 μm to ± 0.6 μm.7 The increase in depth of focus reached a maximum of about 2.0 D at ± 0.6 μm spherical aberration, and the benefit occurred without degrading image quality.
Treatment planning for PRESBYOND requires measurement of spherical aberration. Because the procedure alters the SA in the cornea and does not affect the lens, it is imperative that the total spherical aberration is measured and not just spherical aberration of the cornea. In addition to the existing spherical aberration, the individual PRESBYOND treatment plan considers the functional age of the eye and preoperative refraction (myopia or hyperopia). It is recommended that surgeons develop their own nomogram for each optical zone. In the case described above, the patient was treated with an optical zone of 6.5 mm. Using the clinic's own nomograms, the target refraction and spherical aberration of ± 0.3 μm to 0.6 μm was achieved.
Conclusion
Successful management of presbyopia with high patient satisfaction and reduction of spectacle dependence can be optimized through a personalized approach to select the right modality for each individual. PRESBYOND has the potential to be a safe and effective method of treating presbyopic patients that offers the benefits of a rapid bilateral simultaneous LASIK procedure with focused vision over a range of distances to reduce spectacle dependence. Obtaining an accurate refraction of the patient is fundamental to the success of PRESBYOND, as it is for every LASIK procedure. Achieving the best outcome also requires attention to measurement of total (whole eye) spherical aberration, preoperative testing of eye dominance and anisometropia tolerance, and selecting the proper optical zone for the ablation.
References:
1 Reinstein DZ, Ivory E, Chorley A, et al. PRESBYOND Laser Blended Vision LASIK in commercial and military pilots requiring class 1 medical certification. J Refract Surg. 2023;39(1):6-14.
2 Russo A, Reinstein DZ, Filini O, et al. Visual and refractive outcomes following laser blended vision with non-linear aspheric micro-anisometropia (PRESBYOND) in myopic and hyperopic patients. J Refract Surg. 2022;38(5):288-297. Erratum in: J Refract Surg. 2022;38(7):474. PMID: 35536710.
3 Ganesh S, Brar S, Gautam M, Sriprakash K. Visual and refractive outcomes following laser blinded vision using non-linear aspheric micro-monovision. J Refract Surg. 2020;36(5):300-307.
4 Lim DH, Chung ES, Kim MJ, Chung TY. Visual quality assessment after presbyopic laser in-situ keratomileusis. Int J Ophthalmol. 2018;11(3):462-469.
5 Vargas-Fragoso V, Alió JL. Corneal compensation of presbyopia: PresbyLASIK: an updated review. Eye Vis (Lond). 2017; 4:11.
6 Shetty R, Brar S, Sharma M, Dadachanji Z, Lalgudi VG. PresbyLASIK: A review of PresbyMAX, Supracor, and laser blended vision: Principles, planning, and outcomes. Indian J Ophthalmol. 2020;68(12):2723-2731.
7 Rocha KM, Vabre L, Chateau N, Krueger RR. Expanding depth of focus by modifying higherorder aberrations induced by an adaptive optics visual simulator. J Cataract Refract Surg. 2009;35(11):1885-1892.
Dr. Anke Messerschmidt-Roth is Head of the Eye Clinic Study Center of the Phillips University of Marburg, Germany. The author has a contractual or other financial relationship with Carl Zeiss Meditec AG and its affiliates and has received financial support.
Newsletter
Get the essential updates shaping the future of pharma manufacturing and compliance—subscribe today to Pharmaceutical Technology and never miss a breakthrough.